Introduction to Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a condition characterized by the formation of a blood clot in a deep vein, usually in the legs. This condition can lead to serious complications, including pulmonary embolism, where the clot travels to the lungs, potentially causing life-threatening issues. Understanding the symptoms of deep vein thrombosis is crucial for early detection and treatment. FlowCare is dedicated to providing comprehensive information to help you recognize and address this condition effectively.
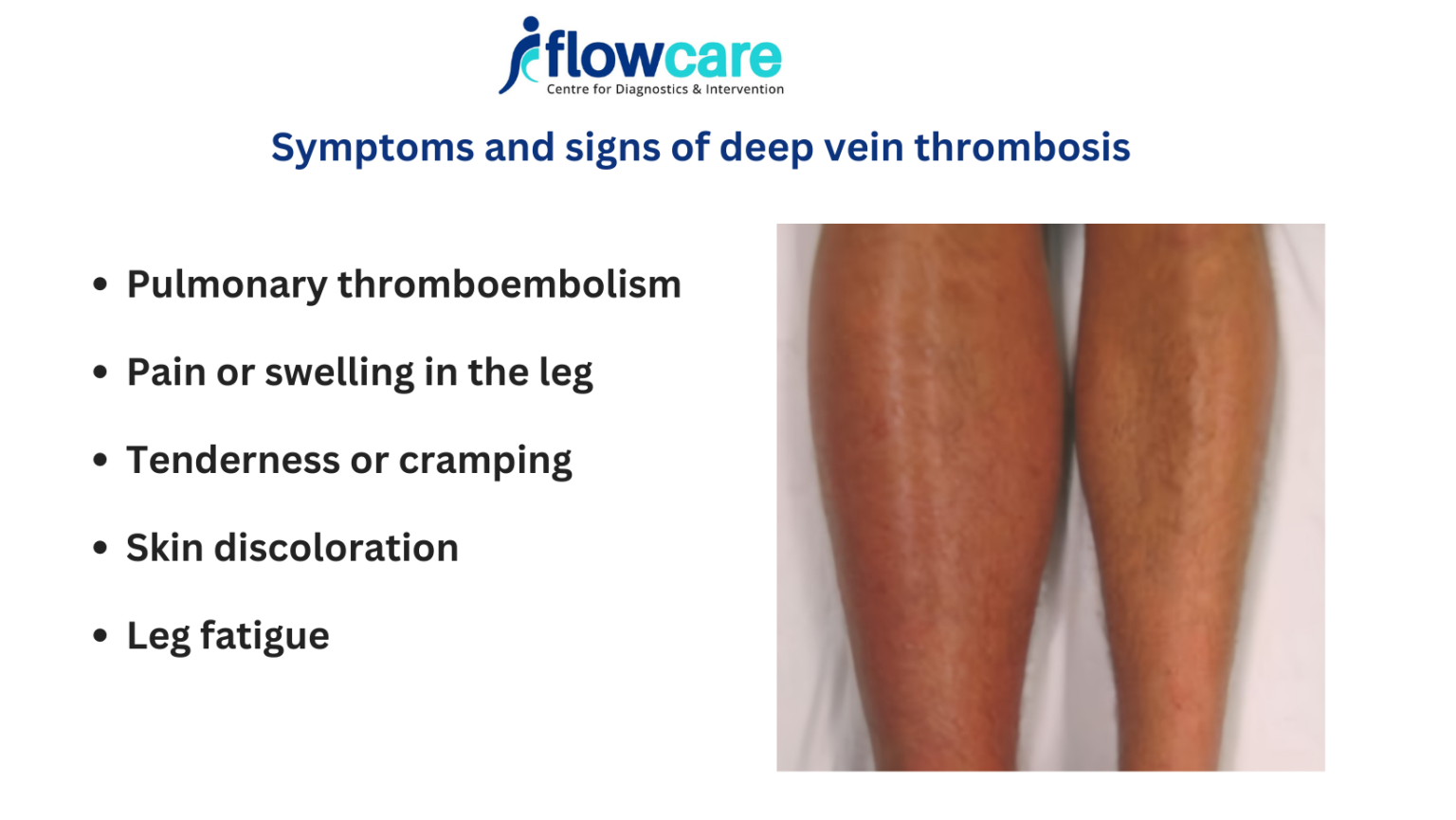
Recognizing Deep Vein Thrombosis Symptoms
Identifying deep vein thrombosis symptoms early can significantly improve the prognosis and reduce the risk of complications. Here are the primary symptoms to watch for:
Swelling in the Affected Limb
One of the most common symptoms of DVT is swelling in the leg or arm where the clot is located. This swelling may occur suddenly and can be accompanied by a feeling of heaviness.
Pain or Tenderness
The pain associated with DVT is often described as a cramping or soreness in the affected area. It usually starts in the calf and can extend to the thigh or arm. The tenderness may be more noticeable when standing or walking.
Warmth and Redness
The skin over the affected area may feel warm to the touch and appear reddish or discolored. This is due to the inflammation caused by the blood clot.
Visible Veins
Sometimes, veins near the surface of the skin become more visible or pronounced, a condition known as superficial thrombophlebitis. This can occur alongside DVT and may indicate an underlying clot.
Shortness of Breath
If a clot breaks free and travels to the lungs, it can cause a pulmonary embolism, leading to sudden shortness of breath, rapid heart rate, and sharp chest pain. This is a medical emergency and requires immediate attention.
Risk Factors for Deep Vein Thrombosis
Several factors can increase the risk of developing deep vein thrombosis. Understanding these risk factors can help in taking preventive measures. FlowCare emphasizes the importance of being aware of the following:
Prolonged Immobility
Long periods of inactivity, such as bed rest or long-haul flights, can lead to blood pooling in the legs, increasing the risk of clot formation.
Surgery and Trauma
Major surgery, particularly involving the pelvis, abdomen, or legs, can increase the risk of DVT. Trauma or injury to the veins can also trigger clot formation.
Medical Conditions
Certain medical conditions, such as cancer, heart disease, and inflammatory bowel disease, can elevate the risk of DVT. Additionally, inherited blood clotting disorders can make one more susceptible to clots.
Hormonal Factors
Hormone replacement therapy and oral contraceptives can increase the likelihood of developing blood clots, particularly in women who smoke or have a history of DVT.
Lifestyle Factors
Obesity, smoking, and a sedentary lifestyle are significant risk factors for DVT. Maintaining a healthy weight, quitting smoking, and regular exercise can reduce these risks.
Preventing Deep Vein Thrombosis
Prevention is a key aspect of managing deep vein thrombosis. FlowCare advocates for the following preventive measures to minimize the risk of DVT:
Stay Active
Regular physical activity, including walking and leg exercises, can help improve circulation and reduce the risk of blood clots. Avoid prolonged periods of sitting or standing still.
Compression Stockings
Wearing compression stockings can help prevent blood from pooling in the legs, especially during long flights or periods of immobility.
Hydration
Staying well-hydrated helps maintain proper blood flow and reduces the likelihood of clot formation. Drink plenty of water, especially during travel.
Healthy Diet
A balanced diet rich in fruits, vegetables, and whole grains can help maintain a healthy weight and reduce DVT risk factors. Avoid excessive salt and alcohol intake.
Medications
For those at high risk of DVT, doctors may prescribe blood thinners (anticoagulants) to prevent clot formation. Always follow medical advice and adhere to prescribed medications.
Diagnosing Deep Vein Thrombosis
Early diagnosis of deep vein thrombosis is crucial for effective treatment. FlowCare outlines the common diagnostic methods used by healthcare professionals:
Ultrasound
This non-invasive test uses sound waves to create images of the blood flow in the veins, helping to detect clots. It is the most commonly used method for diagnosing DVT.
D-Dimer Test
This blood test measures the presence of a substance released when a blood clot breaks up. Elevated levels can indicate the presence of an abnormal blood clot.
Venography
In this invasive procedure, a contrast dye is injected into a large vein, and X-rays are taken to visualize the veins and detect clots.
MRI or CT Scans
These imaging tests can provide detailed images of the veins and are used in cases where ultrasound results are inconclusive.
Treating Deep Vein Thrombosis
Effective treatment of deep vein thrombosis involves managing symptoms, preventing clot extension, and reducing the risk of complications. FlowCare provides an overview of the common treatment options:
Anticoagulants
Blood thinners such as heparin and warfarin are commonly prescribed to prevent existing clots from growing and new ones from forming. Newer anticoagulants like rivaroxaban and apixaban are also used.
Thrombolytics
In severe cases, thrombolytic agents may be administered to dissolve clots quickly. This treatment carries a higher risk of bleeding and is typically reserved for life-threatening situations.
Compression Therapy
Wearing compression stockings helps reduce swelling and prevent further clot formation. This therapy is often recommended alongside medication.
Filter Placement
In cases where anticoagulants are not suitable, a filter may be placed in the inferior vena cava (IVC) to prevent clots from reaching the lungs.
Lifestyle Modifications
Long-term management of DVT includes lifestyle changes such as regular exercise, weight management, and smoking cessation to reduce recurrence risk.
The Importance of Follow-Up and Monitoring
Regular follow-up and monitoring are essential components of managing deep vein thrombosis. FlowCare emphasizes the need for continuous medical supervision to ensure effective treatment and prevent complications:
Regular Check-Ups
Schedule regular appointments with your healthcare provider to monitor the effectiveness of treatment and make any necessary adjustments.
Medication Adherence
Adhere strictly to prescribed medications and report any side effects or concerns to your doctor promptly.
Monitoring Symptoms
Stay vigilant for any changes in symptoms or new signs of clot formation. Seek medical attention if you experience sudden swelling, pain, or shortness of breath.
FlowCare’s Commitment to Vascular Health
FlowCare is dedicated to raising awareness about deep vein thrombosis symptoms and providing reliable information to help individuals manage their vascular health effectively. By understanding the symptoms, risk factors, prevention, and treatment options for DVT, you can take proactive steps to protect your well-being and reduce the risk of complications.
Conclusion
Deep vein thrombosis is a serious condition that requires timely recognition and appropriate management. By staying informed about the symptoms and risk factors, and following preventive measures, you can reduce the likelihood of developing DVT. FlowCare is here to support you with comprehensive information and guidance to ensure your vascular health remains in optimal condition. Always consult with a healthcare professional for personalized advice and treatment options.




